If you have been researching fertility treatment and IVF (In Vitro Fertilization), you may have come across the term “Follicle.” A follicle refers to a tiny fluid-filled sac, inside the woman’s ovary, that contains an egg. You may be wondering how follicle count affects IVF success and how many follicles you will need to be successful in an IVF cycle.
To answer that, let’s take a quick look at how ovarian reserve affects fertility treatment.
Every baby girl is born with all the eggs she’ll ever produce. These eggs mature and ovulate one by one, when she starts her menstrual cycle. As she gets older, her total egg count begins to decline. At a certain age she’ll have very few eggs left. The number of eggs she has remaining at a given time, is called ovarian reserve. Ovarian reserve testing gives an expected number of eggs available. Ovarian reserve testing can help determine the patient’s fertility potential. These numbers can vary dramatically per person by age, history and diagnosis.
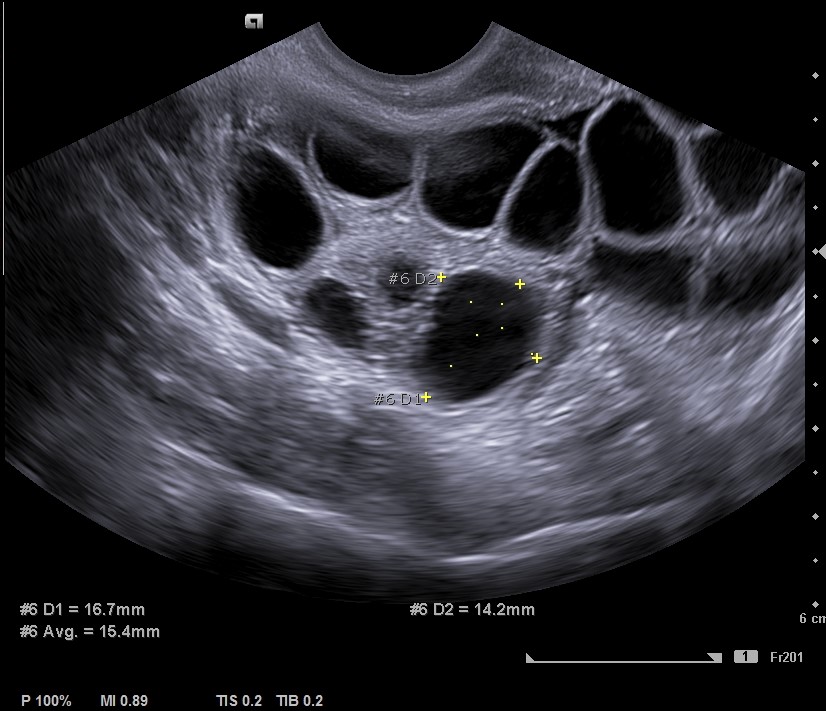
A woman’s ovarian reserve can be estimated by looking at her antral follicle count (AFC). Antral follicles are tiny, fluid-filled sacs inside of the woman’s ovaries. Each of these small sacs houses an immature egg that can be stimulated to produce a mature egg. Using transvaginal ultrasound at the beginning of the menstrual cycle, these “resting follicles” can be observed and counted, which is crucial since follicle count affects IVF success. A high antral follicle count indicates a larger quantity of eggs available, while a lower number may indicate decreasing fertility potential. Ovarian reserve testing can help your provider make recommendations on how to meet your family goals and set appropriate expectations.
During an IVF cycle, the ovaries are stimulated with medications to produce multiple mature eggs. If ovarian reserve is low, not very many eggs will be available to stimulate. Fewer mature eggs to fertilize means fewer healthy embryos to transfer and a lower chance of IVF success. Alternatively, a high antral follicle count could indicate Polycystic Ovarian Syndrome (PCOS). This condition could lead to rare complications such as Ovarian Hyperstimulation Syndrome (OHSS).
But how many is “enough”?
Counting antral follicles is not an exact science, and the experience of the sonographer will affect how many he or she sees. That said, a count of 15 to 30 antral follicles generally indicates a good likelihood of success.
However, the antral follicles don’t tell the whole story. The number of mature follicles that develop will also help determine the likelihood of success. Most fertility clinics like to see multiple mature follicles before triggering ovulation for IVF. Again, this is not an exact science; fewer follicles producing high quality eggs may be sufficient.
A recent study, published in Fertility and Sterility magazine, was looking at the minimum number of mature oocytes (eggs) needed to obtain at least one euploid (chromosomally normal) blastocyst according to the age of the female. The study looked at two groups, one group of patients under age 34, and another group of patients 35 years and older. In the patient age 18-34 group, it took an average of 2.6 eggs to create at least one blastocyst. In the patients age 38 group, it took 2.8 eggs and, in the patient age 43 group it took 4.6 eggs.
As you can see, as the patient’s age increased, so did the number of eggs required to create a blastocyst. If we look at the number of eggs it takes to obtain at least one euploid (chromosomally normal) blastocyst, in the age 18-34 group, it took 4.3 eggs, in the age 38 group, it took 6.2 eggs and, in the patient age 43 group, it took 22.8 eggs. The study concludes that the older the patient, the more eggs will be required to create a chromosomally normal embryo.
What if I don’t have enough?
Female age is directly linked to chromosomally abnormal embryo rates, and as women delay motherhood, this has led many women over the age of 35 to seek fertility treatment. Consequently, egg quality and IVF success rates decrease with advancing age, often leaving patients exploring other options for family building. Alternatives to an IVF cycle with the patient’s own eggs, include using an egg donor. Another option is transferring a previously frozen donor embryo. Talk to your fertility specialist about your options.
For personalized guidance and answers to your fertility questions, consider visiting Bluprint Fertility. Our team of experts is here to provide support, discuss your options, and help you navigate your fertility journey with confidence. Contact us today to schedule a consultation and take the next step towards achieving your family goals.