Infertility affects about 1 in 8 couples in the U.S., with male factor infertility contributing to 30% of cases. Fortunately, fertility treatments like IVF provide multiple options to overcome male factor infertility.
What Causes Male Factor Infertility?
Disorders of the Sperm: Low or absent sperm counts, abnormal sperm morphology (shape of the sperm), and decreased motility (movement) all contribute to male factor infertility.
Hormone Dysfunction: If there is a problem with the hormones sent from the brain to the testicles, there can be a disruption in sperm production.
Previous Trauma or Surgery to the Reproductive Organs: Surgical removal of the testicles, or a vasectomy can impact sperm counts.
Genetics: Some disorders like Klinefelter Syndrome or Cystic Fibrosis can affect your ability to reproduce.
Cancer Treatment: Exposure to chemotherapy and radiation may decrease sperm counts.
Lifestyle: What you eat, how often you exercise, and how you manage stress can all impact sperm.
Medications: Medications like Finasteride and Ketoconazole can interfere with sperm production. Some antidepressants can cause sexual dysfunction.
Medical Problems: Underlying conditions like diabetes can impair erection and ejaculation. Previous infections of the reproductive organs, including sexually transmitted diseases can impact fertility.
How Do You Know to Diagnose Male Factor Infertility?
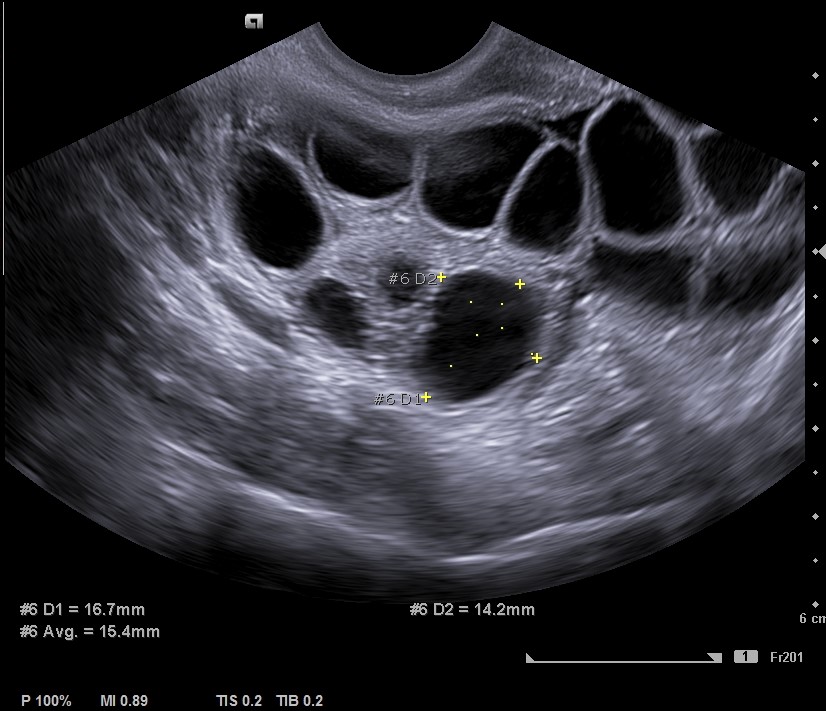
The initial workup for male factor infertility will include a semen analysis. The semen analysis provides important information about a man’s sperm count, motility (movement), and morphology (shape). If the initial analysis comes back with abnormal values, further investigation with a fertility urologist may be recommended. The urologist may go on to order more advanced testing like hormone bloodwork and a scrotal ultrasound. These tests can help diagnose the underlying problem.
Lifestyle Modifications
There are multiple treatment options available to optimize sperm health. In some cases, the quality of the semen can be improved with lifestyle adjustments like diet, weight loss, and stress management. Overall health has a large impact on sperm health, so maintaining a diet full of vegetables, fruits, whole grains, and lean proteins has been found to be beneficial for sperm. Obesity can negatively impact sperm counts, so it is important to incorporate moderate daily exercise to maximize internal testosterone production. Stress can also negatively impact sperm function, so management of stress is important. Yoga, acupuncture, massage, and walking are great ways to reduce stress.
Lastly, raising the body temperature can negatively impact sperm counts. A UCSF study, completed in 2007, evaluated infertile men that had repeatedly been exposed to hot baths, hot tubs, and Jacuzzis at high temperatures. The men were asked to discontinue that exposure for three or more months and 45% of the patients responded favorably to the cessation of heat exposure. They experienced a mean increase in total motile sperm counts of 491% after 3-6 months. High fevers associated with COVID-19, or flu virus can also temporarily impact sperm counts.
Treatment Options for Male Factor Infertility
Treatment options for male factor infertility vary based on severity.
Intrauterine Insemination (IUI)
IUI is an option for mild to moderate cases. The male partner will ejaculate his semen sample into a specimen cup. The sample is then “washed” meaning that dead sperm and debris are removed. The sample is then concentrated into a small amount of fluid. During the insemination procedure, the provider will place the washed sperm sample into a thin catheter and then release the sperm into the female partner’s uterus. IUI shortens the distance the sperm must swim to reach the egg and is timed to occur during the optimal time for conception.
In Vitro Fertilization (IVF)
Another treatment option for mild to moderate male factor infertility is IVF. During an IVF cycle, the female partner’s ovaries are stimulated with medications to promote the production of multiple mature eggs. The eggs are then removed from the body and placed in a small dish with a concentrated amount of sperm. The eggs are closely monitored by the embryologist for the first signs of fertilization.
Moderate to severe cases of male factor infertility may require an additional technique known as Intracytoplasmic sperm injection (ICSI). With ICSI, the embryologist can select a single sperm and inject it directly into the egg. The fertilized egg, now known as an embryo, continues to grow in the lab over the next few days until it is either transferred into a uterus or frozen for future use. ICSI can help couples conceive even when there are very low sperm counts, or even in some cases where sperm is absent from the ejaculate. In severe cases of male factor infertility, a testicular sperm aspiration (TESE/PESA) can be performed by a urologist. A TESE/PESA is a surgical procedure where sperm is extracted from the testicles. The aspirated sperm can then be used in IVF with ICSI.
Here to Help
Dealing with male factor infertility can be challenging, but multiple treatment options are available to help couples on their fertility journey. At Blueprint Fertility, we offer a range of solutions, including IVF for male factor infertility, to address different causes of male infertility, such as sperm disorders, hormonal dysfunction, or genetic issues.
By visiting bluprintfertility.com, you can explore comprehensive diagnostic tools like semen analysis and advanced testing, as well as innovative treatments such as lifestyle modifications, Intrauterine Insemination (IUI), In Vitro Fertilization (IVF), and Intracytoplasmic Sperm Injection (ICSI). Discover personalized plans to overcome infertility and start building the family you’ve always dreamed of!